Arthritis vs. Osteoarthritis: Understanding the Difference

When it comes to joint pain and
inflammation, the terms arthritis and osteoarthritis are often used
interchangeably. However, it's important to recognize that they represent
distinct conditions with different causes, symptoms, and treatment approaches.
In this post, we will explore the key differences between arthritis and
osteoarthritis, shedding light on these common but often misunderstood
conditions.
Arthritis: A General Term for Joint Inflammation
Arthritis is a broad term that encompasses various joint disorders characterized by inflammation. It can affect people of all ages, including children. Some common types of arthritis include rheumatoid arthritis, psoriatic arthritis, gout, and lupus-related arthritis. The underlying causes of arthritis can vary and may include autoimmune diseases, infections, injuries, or wear and tear on the joints over time.
Osteoarthritis: The Most Common Form of Arthritis
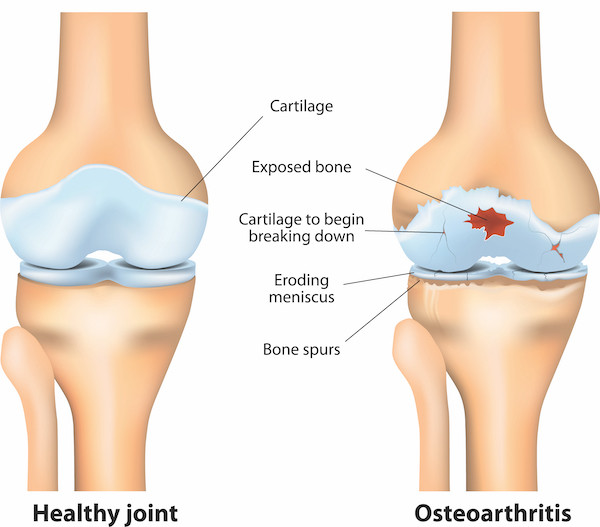
Osteoarthritis, often referred to as degenerative joint disease, is the most prevalent form of arthritis. It primarily affects older adults and is characterized by the degeneration of cartilage in the joints. Cartilage is the smooth tissue that cushions the ends of bones and allows for smooth joint movement. In osteoarthritis, this cartilage gradually breaks down, leading to joint pain, stiffness, and reduced mobility. Weight-bearing joints like the knees, hips, and spine are commonly affected, as well as the hands and fingers.
Causes and Risk Factors
Arthritis can have various causes, including genetic factors, infections, metabolic abnormalities, and an overactive immune system. Osteoarthritis, specifically, is primarily caused by factors such as aging, joint injuries, repetitive stress on joints, obesity, and genetic predisposition. Wear and tear over time contribute to the gradual breakdown of cartilage, leading to the development of osteoarthritis.
Symptoms
The symptoms of arthritis can vary depending on the specific type, but common symptoms include joint pain, swelling, redness, warmth, and limited range of motion. Systemic symptoms such as fatigue, fever, and weight loss may also be present in certain types of arthritis. In contrast, osteoarthritis symptoms typically include joint pain that worsens with activity, stiffness after periods of inactivity, swelling, and a reduced range of motion. Some individuals with osteoarthritis may also experience joint crepitus, which is a grating or cracking sensation during joint movement.
Diagnosis and Treatment
Diagnosing arthritis and osteoarthritis usually involves a combination of medical history, physical examination, imaging tests (such as X-rays or MRIs), and sometimes blood tests to rule out other conditions. Treatment approaches for arthritis aim to manage symptoms, reduce inflammation, and improve joint function. They may include medications (such as nonsteroidal anti-inflammatory drugs and disease-modifying antirheumatic drugs), physical therapy, occupational therapy, lifestyle modifications (such as weight management and regular exercise), assistive devices, and, in severe cases, surgery.
In the case of osteoarthritis, treatment focuses on pain relief, improving joint function, and slowing the disease's progression. Therapeutic options include exercise programs, weight management, pain relievers, corticosteroid injections, physical therapy, and, in severe cases, joint replacement surgery.
Conclusion
While arthritis and osteoarthritis are often used interchangeably, they represent different conditions with distinct causes, symptoms, and treatment approaches. Arthritis is a general term for joint inflammation, whereas osteoarthritis specifically refers to the degeneration of cartilage in the joints. Understanding these differences is essential for accurate diagnosis and effective management. If you experience joint pain or suspect you may have arthritis, consult with a healthcare professional


